ASTMH 2017 Poster - Socioeconomic factors associated with adherence to community directed treatment with ivermectin in onchocerciasis-endemic regions of Ghana
Poster presented at ASTMH 2017 by Simon J. O'Hanlon, Isaac Osei-Akoto, George Domfe, Robert A. Cheke, Mike Y. Osei-Atweneboana, Martin Walker, Maria-Gloria Basáñez
Introduction
Ghana was one of the first countries in West Africa in which community trials of ivermectin (IVM) were conducted and distribution started in the late 1980’s.
Despite many years of mass IVM administration, onchocerciasis transmission persists in many areas and sub-optimal responses to the drug have been reported.
Study Aim
To identify socio-economic factors associated with adherence to community directed treatment with ivermectin (CDTI) in Ghana. In this study, adherence was defined as short-term compliance with CDTI, i.e. at the previous treatment round, and classified as ‘Good’, ‘Random non-compliance’ or ‘Systematic non-compliance’.
- Suboptimal responses to IVM
- Suboptimal responses (SORs) to IVM have been reported in some communities in Ghana (measured as faster rates of microfilarial reappearance in the skin following treatment).
- Some of these communities were first to receive IVM in 1987.
- SORs are of serious concern as IVM is the only drug currently licensed for the treatment and control of onchocerciasis.
- Prior study2 found no apparent association between SORs following treatment and:
- number of treatment rounds previously received
- therapeutic coverage in the village of residence
- infection intensity prior to treatment
Treatment adherence is a crucial determinant of the feasibility of onchocerciasis elimination with IVM. The factors associated with adherence to treatment have not been investigated in Ghana.
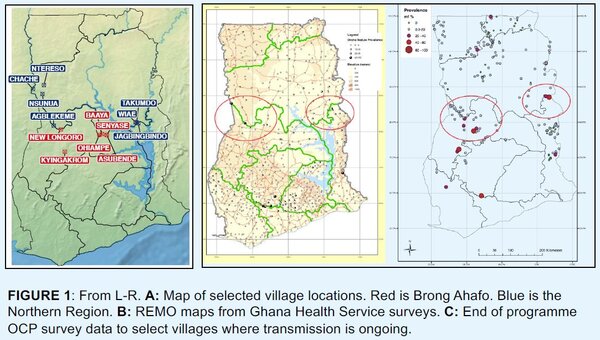
Site selection and survey instrument
- Villages mostly selected from the study by Osei-Atweneboana et al. (2007)1
- 7 villages had mf repopulation rates indicating normal response to IVM
- 3 villages had sub-optimal responses to IVM (Kyingakrom, New Longoro and Jagbenbendo [Jagbingbindo in Figure 1A])
- Using GIS and parasitological survey data, a number of potential ‘transmission hotspots’ were identified (Figure 1C) where ongoing transmission was deemed a problem, identifying 3 further villages
- 13 communities in the Brong-Ahafo and Northern regions of Ghana (Figure 1B) were surveyed, collecting detailed socio-economic and health information
- Hierarchical, random sample questionnaire was administered to 280 households (40 households in New Longoro due to community size)
Results
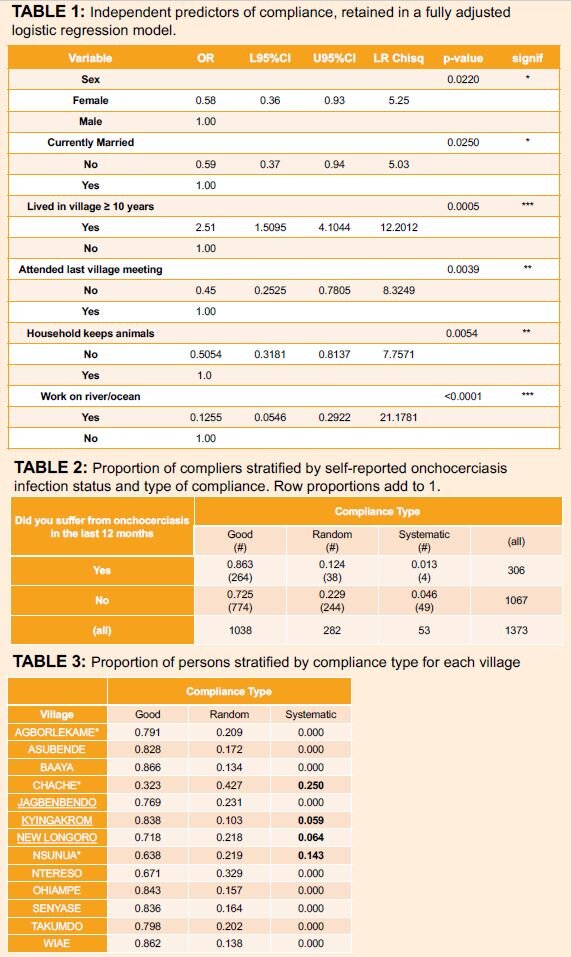
A total of 1,383 people were interviewed in 280 households, across 13 villages from Jun 2011 to Jan 2012. Systematic non-compliers were more likely to self-report as ‘uninfected with onchocerciasis’. Six factors were identified to be statistically significantly positive predictors of adherence to ivermectin treatment:
- Being male.
- Being currently married.
- Residing in the village for 10 years or more.
- Having attended the last village meeting.
- Being involved in domestic animal husbandry.
- Main place of work being neither near the river nor the lake.
Discussion
- Similar studies have been undertaken in formerly APOC countries, e.g. Ethiopia, Nigeria, Cameroon, Uganda
- These are the first data on predictors of adherence in the West African setting of the former Onchocerciasis Control Programme
- 4 villages were identified with systematic non-compliers, ranging from 6% to 25%, 2 of which previously identified as being ‘of concern’ due to SORs
- Statistically significantly faster rates of skin repopulation following treatment in Jagbenbendo, Kyingakrom and New Longoro, even after biannual treatment
- SORs in Kyingakrom and New Longoro might be partially explained by levels of systematic non-compliance
- Chache: high proportion of systematic non-compliers. Mainly rehoused families due to Bui National Park dam development who did not choose their own community drug distributor (CDD)
- Ntereso: the other community which did not choose their own CDD (33% of random non-compliers)
- Electing their own CDDs may be an important factor for community members adhering to CDTI
References
- Osei-Atweneboana et al. (2007) Prevalence and intensity of Onchocerca volvulus infection and efficacy of ivermectin in endemic communities in Ghana: a two-phase epidemiological study. Lancet 369: 2021-
- Churcher et al. (2009) Identifying sub-optimal responses to ivermectin in the treatment of River Blindness. Proc Natl Acad Sci U S A 106:16716-21.
- Endale et al. (2015) Predictors of compliance with community-directed treatment with ivermectin for onchocerciasis control in Kabo area, southwestern Ethiopia. Parasit Vectors 8: 99.
- Brieger et al. (2012) Characteristics of persons who complied with and failed to comply with annual ivermectin treatment. Trop Med Int Health 17: 920-30.
- Oyibo & Fagbenro-Beyiku (1998) Evaluation of community compliance with annual ivermectin treatment of onchocerciasis in Patigi, Nigeria. East Afr Med J 75: 237-42.
- Brieger et al. (2011)Compliance with eight years of annual ivermectin treatment of onchocerciasis in Cameroon and Nigeria. Parasit Vectors 4: 152.
- Nuwaha et al. (2004) Predictors for compliance with community directed ivermectin treatment in Bushenyi district of Uganda: qualitative results. East Afr Med J 81: 92-96.
- Nuwaha et al. (2005) Predictors of compliance with community-directed ivermectin treatment in Uganda: quantitative results.. Trop Med Int Health 10: 659-67.
- Frempong et al. (2016) Does Increasing Treatment Frequency Address Suboptimal Responses to Ivermectin for the Control and Elimination of River Blindness? Clin Infect Dis 62:1338-47.